Hypospadias is a congenital defect with an abnormal urinary opening and is usually associated with downward bending of the penis which is called as chordee. Surgery is required to correct the hypospadias in which the urinary opening is brought to the tip of the penis, curvature is straightened, and skin is rearranged to give a circumcised appearance. Certain things are to be avoided after hypospadias surgery to avoid stress on the surgical site and ensure proper healing. Here are the things which are to be avoided after hypospadias surgery:
1. Activity and bathing restrictions:
Straddle toys and activities: Any activity which puts pressure in the penile area should be avoided after surgery for a period of 4 weeks. This includes riding bicycle, riding toy horse, see-saw, swings etc. Any activity that involves spreading the legs can apply pressure on the penile area.
Sports: Any sport activity involving ball which can cause impact on the penile area should be avoided.
Swimming: Swimming should be avoided for 6 weeks after hypospadias repair. Public or natural water sources (chlorinated pools) contain bacteria, chemicals and contaminants that can lead to serious wound infection because the surgical site is a fresh healing wound.
Bathing: Avoid soaking the hypospadias dressing or wetting it till it is removed. Sponge bath is recommended till the dressing and catheter is present. Start bathing the child once your doctor has given the green signal. Bath is allowed once dressing and catheter is removed but soap application and rubbing the penile area should be avoided for 3 weeks after dressing removal.
2. Hypospadias Wound and Dressing care:
Dressing care: Dressing should be kept clean and avoid soiling of dressing with stool. If dressing gets dirty, it must be changed. If dressing is completely soiled with stool, then dressing is removed, betadine wash is given, and operated site is left open till catheter removal.

Pic 1: Clean dressing after hypospadias surgery
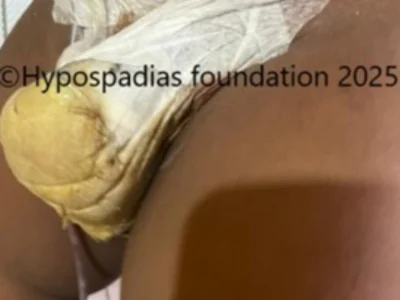

Pic 2: Soiled dressings in the post operative period after hypospadias surgery
Catheter handling: A urinary tube is kept after hypospadias surgery to drain the urine. This tube should be handled carefully till removed. Pulling/ pushing of the tube should be avoided because it can cause stress on the newly reconstructed urethra. Also, the end of the tube which drains urine should be kept clean to avoid infection.
Avoid constipation: Straining while passing stool after surgery can cause pressure on the operated site in turn putting stress on the stitches which may lead to giving away of the stitches causing dehiscence (opening of the operated site). Hence avoid constipation in the post-surgery period. If the child has constipation, pls inform the doctor so that a laxative can be prescribed at time of discharge.
Operated site care: Once the dressing and catheter is removed, sitz bath is started. Sitz bath is soaking the operated area in lukewarm water. We advise parents to make their children sit in the bathtub for 3-5 minutes, three times daily after dressing and catheter removal. After cleaning the area, it should be dried. Avoid using cotton, wet wipes or rubbing the area. Only pat dry the area gently, alternatively you can put the diaper on wet penis. The diaper will absorb the water and the wound will become dry. Once dried ointment should be applied 2-3 times daily for 2-3 weeks depending on the healing. Presence of swelling, bruising and redness are normal after hypospadias surgery, and they gradually reduce after 2 weeks. The penis may look crooked and bent due to the swelling. There is no need to panic if the child is passing urine well.
3. Do not stop or miss the medicines:
Medicines are to be continued as per the doctor’s advice. Do not stop the antibiotics or other medicines prematurely in the presence of urinary tube because it can lead to infection.
Always follow the specific post operative instructions given by your doctor. This instruction will vary slightly depending on the type of repair, post operative healing and the surgeons preference.
At hypospadias foundation, we provide detailed post-surgery instructions, which are vital for a successful recovery. With an experience of more than 5000 hypospadias surgeries, we have protocols in place for management of post operative dressing and catheter care. Dr Singal and Dr Shenoy with their vast experience have developed good post operative care regimen which is easy for parents to follow. Good post-surgery care will cause good healing of the operated site and will decrease the risk of complications.
Dr A.K. Singal is a highly respected and experienced Pediatric urologist and hypospadias specialist in India. He is widely recognized for his expertise in surgical treatment of hypospadias and considered as the best hypospadias surgeon in India and the world. He has developed innovative surgical techniques and treatment algorithms particularly for complex and failed cases, with strong emphasis on achieving successful functional and cosmetic outcomes.
Dr Shenoy specializes in pediatric urology and hypospadias providing advanced surgical techniques for both primary and failed hypospadias repair in children and adults. Their combined experience and shared focus on a single, complex condition contribute to the foundation’s high success rate.
Contact Form for Hypospadias Foundation
Please fill all clinical details and upload pictures and clinical summaries (if available)