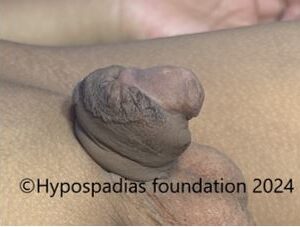
2 year 6 months male child came to Hypospadias Foundation from Nepal with complaints of passing urine from the mid penile region associated with abnormal ventral curvature of the penis. Parents were looking for an experienced hypospadias surgeon hence they delayed the surgery till 2.5 years of age. On examination, the meatus was in the mid penile region with poor urethral plate. He was planned for hypospadias repair, and we counselled the family that whether the surgery would be in 1 stage or two stages will be decided depending on the degree of chordee during surgery.
At the start of hypospadias surgery, the entire penile skin was taken down all around till the base of the scrotum, a step known as complete degloving. Chordee was assessed after complete degloving. Chordee was noted to be more than 45 degrees. This was because of deficient tissues on the underside of the penis. We made a horizontal incision on the underside of the penis at the site of maximum curvature and divided the urethral plate. After division of the urethral plate, the proximal urethra was mobilized. Chordee was reassessed and there was persistent chordee of more than 30 degrees noted. Site of maximum curvature was marked on the ventral side. Three Corporotomies were done by placing horizontal incisions ventrally over the tunica with middle incision at the site of maximum curvature. Chordee was reassessed and less than 30-degree chordee was noted. Complete Chordee correction was achieved by tunica albuginea plication at 12’o clock position on the dorsal side. Artificial erection test showed straight penis.
After that the foreskin(prepuce) was divided in the midline and rotated to cover the underside of the penis- a step known as Byar’s flaps. This hairless prepucial skin which is now on the underside of penis will be utilized in the second stage for urethroplasty.

Picture 1: On clinical examination, the meatus was at the mid penile region with severe chordee


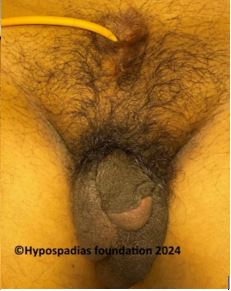
Picture 2: Marking done for degloving and complete degloving done


Picture 3: Artificial erection test was done which showed chordee of more than 45 degrees and hence urethral plate division was done


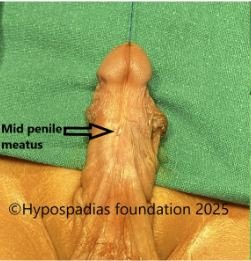
Picture 4: Persistent chordee of more than 30 degrees hence three ventral corporotomies given


Picture 5: Less than 30 degrees chordee noted after three ventral corporotomies hence 12’o clock dorsal tunica albuginea plication done. No chordee after dorsal tunical plication


Picture 6: Dorsal prepuce(foreskin) divided in the midline and rotated to cover the underside of the penis
Second stage of Hypospadias Repair:
After 6 months of first hypospadias surgery, the child was taken up for second stage urethroplasty. We checked chordee again- the penis was completely straight. The prepucial flaps which were done in first stage had healed very well. The flaps were wide and supple. 15mm wide incision was marked on the flaps and, local anaesthesia was infiltrated at the marked site and incisions were deepened till corpora and hemostasis checked. Urethroplasty was done over 7Fr Infant feeding tube in two layers with 6-0 PDS absorbable sutures. Glans wings were raised, Glansplasty was done, and a new meatus was made on the glans. The dressing in the post operative period was changed on post operative day 7 and catheter was removed on post operative day 10. Child was passing urine through the new opening in good stream.


Picture 7: Prepucial flaps 6 months after stage 1 were healed very well. Flaps were wide and supple.

Picture 8: Artificial erection test done – completely straight penis noted


Picture 9: Urethroplasty done over 7Fr Infant feeding tube and dartos flap raised on both sides


Picture 10: Glans wings raised, distal urethroplasty done and Dartos flap sutured over the urethroplasty.

Pic 11: Glansplasty and skin closure done, completing Stage 2 urethroplasty

Pic 12: Post catheter removal, passing urine in single straight stream with no complications.
Two stage repair in hypospadias with severe chordee
Staged repair in hypospadias is a preferred approach in cases of severe hypospadias when the urethral opening is significantly displaced and there is significant chordee. Two stage repair involves two separate surgeries to correct the hypospadias, the first stage being correction of the bend of the penis and rearranging the foreskin on the underside of the penis. The second stage is usually performed 6-12 months after stage 1 hypospadias repair.
Two stage repairs are often considered to offer superior functional and cosmetic results in severe hypospadias compared to attempting a single stage complex repair. They allow for a
more controlled approach to address significant curvature and create a neourethra with potentially better tissue quality from the prepucial flaps. Whether your child needs a single stage repair or a staged approach is best decided by the expert hypospadias surgeon during the initial steps of surgery and is primarily dictated by the degree of curvature.
About Hypospadias foundation
Hypospadias foundation is an organization dedicated for children and adults with hypospadias and is rated as the best hospital for hypospadias repair in India and the World. Hypospadias foundation offers best results for surgical repair for primary and failed(redo) hypospadias. We at hypospadias foundation believe in providing personalized care and psychosocial support to families of children and adults with hypospadias. Dr A K Singal is a well renowned hypospadias surgeon and regarded as the best hypospadias surgeon in India and in the world. His vision for hypospadias has helped him achieve excellent outcomes in adults and children with hypospadias. He has dedicated his life in treating children and adults with hypospadias with his innovative surgical techniques. Dr Ashwitha Shenoy is an expert pediatric surgeon with special interest in pediatric urology and hypospadias. She holds a particular interest in hypospadias and along with Dr Singal performs advanced surgical techniques for both primary and complex hypospadias cases in children and adults.