Hypospadias is a congenital condition where the opening of the urethra (where urine and semen exit) is not at the tip of the penis but somewhere along the underside of the penis. The location of the opening can vary from a mild one (near the tip) to a severe one (at the base of the scrotum). Nearly 70% of all hypospadias also have an associated penile curvature where the penis bends downwards, known as chordee. Hypospadias repair surgery is typically performed between 6-18 months of age. A successful hypospadias surgery aims to reposition the urethral opening to the tip of the penis, straighten the penile curvature and align the skin to give a final circumcision type of cosmetic outcome.
When it comes to fertility in men, penis and testis play a crucial role. Here is a detailed information on how hypospadias can have an impact on fertility:
1. Production of semen:
In isolated cases of hypospadias with normal testes, the sperm production is not impacted, and fertility is normal. But upto 10% of patients with hypospadias may have associated undescended testis, and this association is mostly present in severe hypospadias. Testis is the core organ for male fertility. It produces sperms and male sex hormone called as testosterone. Testosterone is essential for development of penile growth. Both sperm production and testosterone production will be impacted if the testis is not functioning fully. Hence if the person has both hypospadias and undescended testis, there may be an impact on fertility, especially if there was undescended testis on both sides. In these cases, where we have both hypospadias and undescended testis, we need to investigate for DSD (Disorder of sex development) which is seen in 15% of such cases.
2. Presence of penile curvature:
While mild chordee may not impair sexual activity, presence of chordee more than 30 degree can make sexual activity difficult and painful. Hence straightening of the penis (chordee correction) is a very crucial step in hypospadias repair.


Chordee assessed by artificial erection test and less than 30-degree chordee noted, corrected by 12’o clock dorsal tunica albuginea plication (TAP)


Chordee more than 30-degree, corrected by urethral plate division, proximal urethral mobilization and 12’o clock dorsal tunica albuginea plication (TAP)


Chordee noted to be more than 60-degrees, corrected by urethral plate division, proximal urethral mobilization, three ventral corporotomies and 12’o clock dorsal tunica albuginea plication (TAP)


Severe chordee with ventral curvature of more than 90 degrees, corrected by urethral plate division, proximal urethral mobilization, three ventral corporotomies and ventral lengthening procedure – dermal graft.
3. Problems with ejaculation in hypospadias:
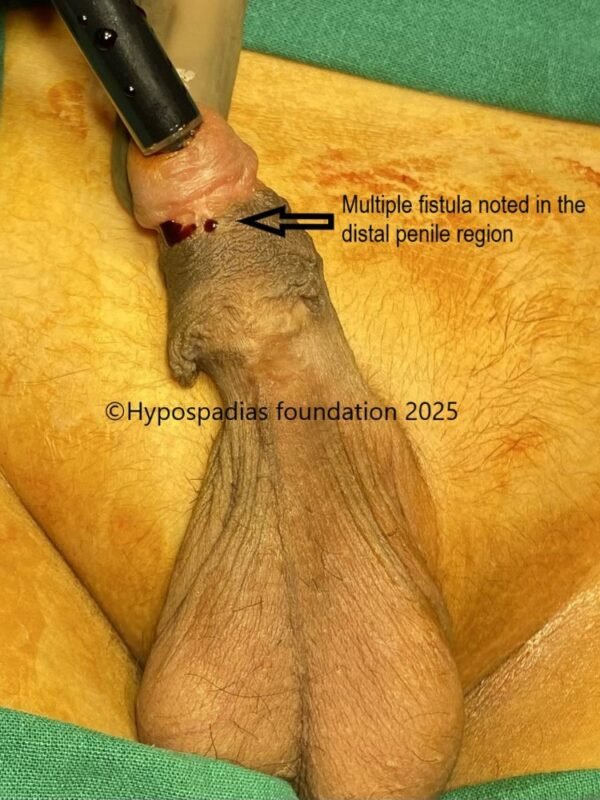
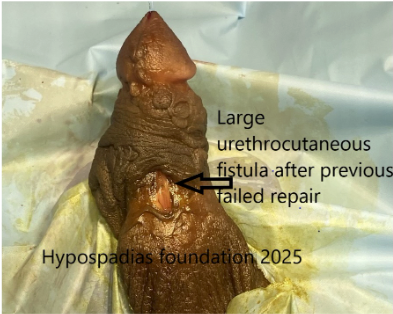
In uncorrected hypospadias with urinary opening located far below on the shaft of the penis or near the scrotum, the sperm may not deposit correctly in the vagina. Also, if the hypospadias repair has not healed properly leading to a narrow urethra (stricture urethra) or loose and bulged out urethra (severe urethral diverticulum), the semen may not ejaculate with good force. Failure of semen to reach the vagina is the cause of infertility in these cases. Hypospadias repair is essential in these patients to bring the opening to the tip of the penis and reconstruct the narrow or bulged part to allow for proper ejaculation.
4. Psychological impact:
Uncorrected Hypospadias or failed hypospadias can have psychological impact on individuals affecting their quality of life, self-esteem, social interactions when transitioning from childhood into adulthood. Adults who had hypospadias repair in childhood have reported being more timid and more isolated in childhood. In spite of successful hypospadias repair, some individuals may feel that their genitalia look different from others, leading to feeling of inadequacy and shame. This can make relationships with the opposite gender difficult and hence may be an indirect cause of infertility. Hence our advice to parents of children with hypospadias is that they should provide information about hypospadias and disclose it to their child so that they know why their penis will look different from others. This disclosure is best done during puberty between 12-15 years of age because the boys will understand the situation better at this age. Often parents bring the boys around puberty to our hypospadias centre and then we also discuss and provide full information to the boys in front of their parents. Once they are aware, accepting the situation will help them gain confidence and develop in their sexuality and also prevent any negative feelings of inadequacy.
Key message for parents
If your child has isolated hypospadias then post successful hypospadias surgery by an expert hypospadias surgeon, most likely he will not suffer from infertility in adulthood. Hence early identification, timely surgical intervention is necessary to treat the physical challenges which could impede fertility. After a successful hypospadias surgery, the ability to perform intercourse and have a normal ejaculation will significantly improve the ability to have a child.
Even after a successful hypospadias repair if an adult has difficulty conceiving, then he needs to consult a hypospadias surgeon to make sure that the previously reconstructed urethra is normal followed by a fertility specialist for further evaluation to rule out other causes of infertility. With modern surgical techniques and medical care, even a boy with severe hypospadias can lead a normal adult life and have children.
About Hypospadias Foundation
Hypospadias foundation is a specialized centre in India dedicated to the care and treatment of children and adults with hypospadias and related conditions. It is located in Kharghar, Navi Mumbai, Maharashtra. The foundation’s sole focus on a single condition hypospadias allows them to develop specialized techniques and protocols aimed at achieving the best possible outcomes for their patients. Their success rate for hypospadias correction surgery is more than 95% making them one of the top centres in the world for hypospadias repair.
Dr A.K. Singal is a highly respected and experienced Pediatric urologist and hypospadias specialist in India. He is widely recognized for his expertise in surgical treatment of hypospadias and considered as the best hypospadias surgeon in India and the world. He has developed innovative surgical techniques and treatment algorithms particularly for complex and failed cases, with strong emphasis on achieving successful functional and cosmetic outcomes.
Dr Shenoy specializes in pediatric urology and hypospadias providing advanced surgical techniques for both primary and failed hypospadias repair in children and adults. Their combined experience and shared focus on a single, complex condition contribute to the foundation’s high success rate.
Contact Form for Hypospadias Foundation
Please fill all clinical details and upload pictures and clinical summaries (if available)