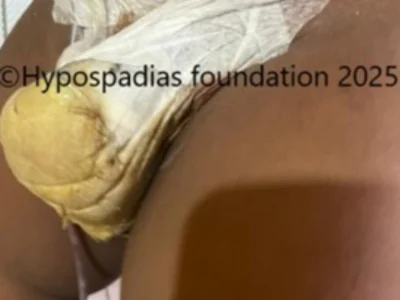
Mast B.E, 14-year male from Mumbai had undergone two unsuccessful hypospadias repairs at another hospital in the past. He presented to Hypospadias Foundation with complaints of passing urine from two sites, which is from the tip and from the distal penile region. On clinical examination, there was an eccentric subcoronal fistula with a thin glans bridge separating it from the glanular meatus. There was some residual skin on the dorsal side. The urine stream was spraying as shown in the photo below
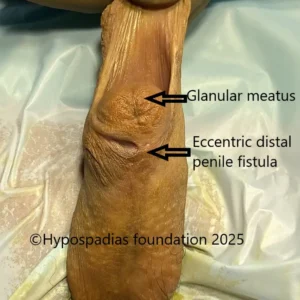

Picture 1: On clinical examination, there was an eccentric distal penile fistula with thin glans bridge separating it from the glanular meatus

Picture 2: Urine stream was poor with spraying of urine.
He was planned for single/ two stage repair depending on the degree of chordee, status of native urethra and quality of urethral plate. Cystoscopy was noted to be normal. Chordee assessment showed no residual chordee. The thin glans bridge between the meatus and the fistula was divided. The urethral plate was noted to be wide with no scarring. Considering all the above factors he was planned for single stage repair – simple tube urethroplasty or Glans Approximation Procedure was decided.


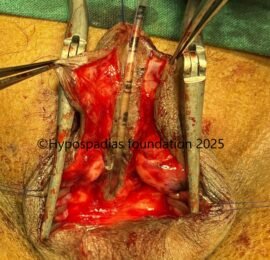
Picture 2: Artificial erection test showed no residual chordee. Urethral plate was noted to be wide and healthy.
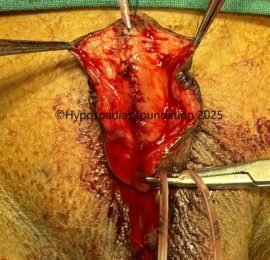
Stay suture was taken on the glans with 4-0 prolene. Complete degloving was done. Artificial erection test showed no residual chordee. Glans wings were marked and raised. Urethroplasty was done by continuous inverting subcuticular sutures with 6-0 PDS over 8Fr infant feeding tube. Second layer closed over the urethroplasty with local tissues with 6-0 PDS interrupted sutures. Right dartos flap was raised and sutured over the urethroplasty with 6-0 PDS. Glansplasty was done with 5-0 vicryl. Unhealthy skin was excised; edges were freshened and closed in 2 layers with 6 0 PDS and 6-0 vicryl rapide.


Picture 3: Complete degloving done and chordee assessed by artificial erection test. No chordee noted.


Picture 4: Urethroplasty done with 6-0 PDS, followed by glansplasty and skin closure


Picture 5: Appearance and urine stream at 2 weeks after catheter removal

Picture 6: Follow up at 6 months after surgery
Click here to watch the entire video of this surgery
Redo urethroplasty for a distal urethral fistula – Hypospadias Foundation, India
Redo urethroplasty for failed hypospadias
Redo urethroplasty for failed hypospadias is a highly complex and challenging surgical procedure. The primary goal is to address the complications of the initial surgery which are often associated with tissue scarring, shortage of tissues and presence of residual chordee. The general goals for any redo urethroplasty are to straighten the penis (correct any residual chordee), to reconstruct the urethra (create
a new wide and patent urinary passage) and place the urinary opening at the tip of the penis (glanular meatus).
Redo hypospadias repair should be performed by a experienced pediatric urologist or hypospadias surgeon who has expertise in complex hypospadias repairs. Surgeon should wait atleast 6 months after the initial repair to allow the inflammation to subside and for the scar tissue to soften. Sometimes if there is significant scarring, we wait for even 1-2 years and use steroid creams to soften the scar area.
About Hypospadias Foundation
Hypospadias Foundation is a centre specialized for treatment of children with hypospadias. It is located at MITR hospital, Kharghar, Navi Mumbai in the state of Maharashtra, India. Our expertise in primary and redo hypospadias repair makes us one of the best centres for hypospadias treatment in the world. We get children from more than 30 countries in the world with various types of complications after hypospadias surgery done at other centres and we are able to repair them successfully with good cosmetic outcomes. This is possible because of our dedication in the field of hypospadias.
Dr A K Singal is an expert and top hypospadias surgeon in India. He is a gifted surgeon and his expertise in this area has helped us achieve excellent outcomes in primary and failed hypospadias in children as well as adults.
Dr Ashwitha Shenoy is an expert hypospadias surgeon with special interest in hypospadias and pediatric urology. Both Dr Singal and Dr Shenoy work together to give best results for hypospadias surgery in India for both children and adults.
Single stage hypospadias repair in a child with recurrent distal penile fistula
A urethral fistula after hypospadias repair is an abnormal communication that forms between the newly reconstructed urethra and the skin on the underside of the penis. This is the most common complication that occurs after hypospadias surgery. In this condition, the urine comes from the tip of the penis and leaks from the fistula site.
This fistula mostly occurs due to issues with healing of the urethra. The common reasons include tension on the newly reconstructed urethra, poor blood supply at the operated site, gaps during closure, infection at the operated site, narrowing or stricture formation in the new urethra or straining while passing stool in the post operative period.
Children who form fistula after hypospadias surgery come with leaking or dribbling of urine from the fistula site. Symptoms usually appear within a few weeks to months after the initial hypospadias repair.
The primary treatment is surgical repair if they do not close on their own. It is standard practice to wait for atleast 6 months after the initial hypospadias repair before attempting fistula closure. This allows the tissues at the urethral fistula site to soften, improve blood supply and increase the success rate of second surgery. The fistula tract is identified and excised to create healthy tissue edges for repair.
The urethral fistula site is closed in multiple layers as done in the above-mentioned case to ensure a watertight seal and prevent recurrence. Before closing the fistula, it is always necessary to confirm that the urethra beyond the fistula site is not narrow or tight. In the presence of distal obstruction, the urethral fistula closure surgery may fail.
If your child has developed urethral fistula after hypospadias repair, then it’s necessary that you see a hypospadias specialist who will assess what is best for your child and choose the best technique minimizing the risk of complications and improving the chances of success.
About Hypospadias Foundation
Hypospadias Foundation is a centre specialized for treatment of children with hypospadias. Hypospadias foundation is located at MITR Hospital in Kharghar, Navi Mumbai in the state of Maharashtra. Our expertise in hypospadias makes us one of the best centres for hypospadias repair in the world. We treat children from more than 25 countries in the world and from all over India. Our dedication in this field has helped us achieve excellent outcomes.
Dr A K Singal is an expert and top hypospadias surgeon in India. He is a gifted surgeon and his expertise in this area has helped us achieve excellent outcomes in primary and failed hypospadias in children as well as adults.
Dr Ashwitha Shenoy is an expert hypospadias surgeon with special interest in hypospadias and pediatric urology. Both Dr Singal and Dr Shenoy work together to give best results for hypospadias surgery in India for both children and adults.