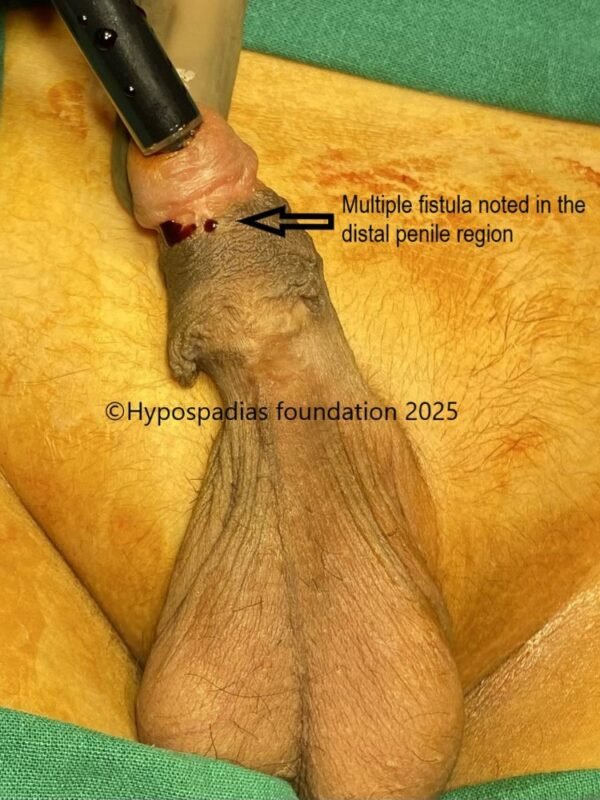
30-year-old male presented to the hypospadias clinic with complaints of passing urine from the distal penile region. He had not undergone any surgery in childhood since his parents were not aware about their child’s hypospadias condition. On examination in the OPD, the meatus was narrow and was in the distal penile region. He also had significant chordee on erection. He was counselled for single or two stage repair depending on the estimation of degree of chordee in the operation theatre.
Stage 1 Repair- Chordee correction and Oral Mucosa graft
The hypospadias repair surgery was started by complete degloving. Artificial erection test after degloving showed more than 45-degree ventral chordee. Since the chordee was significant with the urethra appearing short and taut, the urethra was divided, and proximal urethra was mobilized. Artificial erection test after urethral plate division showed less than 30-degree chordee, hence we decided to correct it by dorsal 16 dot plication procedure.
Buck’s fascia along with neurovascular bundle was raised on the dorsal side starting laterally on either side and upto the midline. Artificial erection test was done, and exact site of maximum curvature was marked on the dorsal side. 16 dots (8 dots on either side) were marked- 4 dots proximal and 4 dots distal to the site of maximum curvature. Longitudinal plication sutures were placed at these sites with 4-0 prolene involving full thickness tunica albuginea. Chordee was completely corrected by these equally spaced plication sutures. Buck’s fascia was closed on either side with 6-0 PDS. Proximal urethral stump was fixed at the proximal penile region. Distal tunical bed was prepared for placement of oral mucosa graft. Glans wings were widely raised.
A long 10cm Oral mucosa graft was harvested from inside of the right cheek and lower lip. Graft was defatted and quilted in the urethral bed with 5-0 vicryl. Pressure dressing was done, and the catheter was fixed to the glans stitch. Dressing and catheter were removed after 7 days.
Graft uptake in this case was 100% with no graft loss. After 21 days, local steroid massages were started and continued till 5 months.
Stage 2 Oral Mucosa Graft Urethroplasty
Graft was soft and supple at 6 months after graft placement. Surrounding skin was also heathy and soft. Urethroplasty was started by marking the edges of the graft. Local anaesthesia was infiltrated at the marked site. U-shaped incision was given at the edges of the graft and was deepened till the corpora. Urethroplasty was done over 14Fr silicone catheter with 5-0 vicryl in 2 layers. Local dartos flap was used for second layer coverage. Skin was closed in 2 layers and dressing was done. Suprapubic cystostomy was done with 14Fr malecot’s catheter. Dressing was
changed on post-surgery day 4 and every 4 th day thereafter. During every dressing change, betadine wash was given, and redressing was done. Per urethral catheter was removed on post operative day 14. Suprapubic catheter was removed on post operative day 21. Patient passed urine in good stream without pain or leak after catheter removal. At 6 months follow up after surgery, the cosmetic result was good, and the patient was passing urine from the glanular meatus in good stream.


Pic 1: On examination, the meatus was noted to be in the distal penile region


Pic 2: Complete degloving was done. Artificial erection test done showed more than 45 degree chordee


Pic 3: Urethral plate was divided, proximal urethra was mobilized and chordee reassessed. Artificial erection test after urethral plate division showed less than 30 degree chordee.


Pic 4: Since the chordee was less than 30 degree, we planned to do 16 dot plication on the dorsal side. Buck’s fascia along with neurovascular bundles were raised and longitudinal plication sutures were placed at 4 points.


Pic 5: 16 dot plication done and chordee was completely corrected. Glans wings were raised

Pic 6: Oral mucosa graft harvested from right cheek

Pic 7: Oral mucosa graft harvested from lower lip

Pic 8: Oral mucosa graft sutured on the ventral aspect of the penis with 5-0 vicryl thus completing the stage 1 oral mucosa graft placement
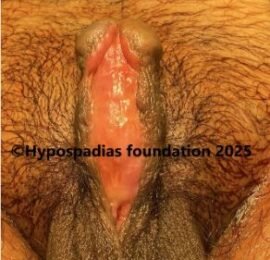

Pic 9: Assessment at 6 months after stage 1 done. Graft uptake was 100% and graft was soft, supple and ready for stage 2 urethroplasty


Pic 10: Marking done at the edges of the graft. Incision given at the edges of the graft and deepened till the corpora.


Pic 11: First layer of urtehroplasty done in continuous subcuticular fashion with 5-0 Vicryl. Dratos flap raised from the left side.


Pic 12: Dartos flap from the left side sutured over the distal urethroplasty and completion of stage 2 urethroplasty


Pic 13: Cosmetic result 6 months after stage 2 showing good outcome and a wide glanular meatus
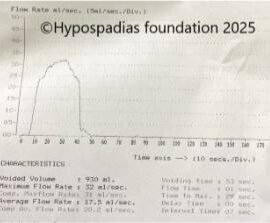
Pic 14: Post surgery uroflowmetry showed normal flow rate
Distal penile hypospadias repair surgery in an adult
Hypospadias is a congenital condition which is present since birth. When not operated in childhood, adults visit our Hypospadias Foundation Clinic for surgical repair in adulthood. The above mentioned case is of a 30 year old male who presented to us with distal penile hypospadias with severe chordee. He was counselled that the decision of single or two stage will be taken during the surgery after assessment of the degree of chordee.
Artificial erection after degloving showed significant chordee and we had to proceed with staged repair. In first stage, the chordee was completely corrected by urethral plate division and dorsal 16 dot plication. We avoid corporotomies in adults because then oral mucosa graft uptake is poor at the sites of deep corporotomy. In adults, the length of oral mucosa graft required is usually long andd hence mostly it needs to be harvested from the cheek and lip. Steroid massages are started on the graft 3 weeks after graft placement.
Second stage is planned 6-8 months after stage 1. Suprapubic cystostomy is a must in all post pubertal and adults undergoing urethroplasty. Post surgery care is extremely important in adults after hypospadias repair. At our centre, we inspect the operated site once every 4 days to make sure that there is no surgical site infection because wound infection after stage 2 can cause dehiscence of the the entire urethroplasty. We remove per urethral catheter first which is around 14 days followed by SPC clamping and removal at 21 days provided there is no dehiscence.
After having done hundreds of adult hypospadias surgeries, we can clearly see differences in adult hypospadias repairs compared to hypospadias repair in a child. Whether it is the size of penis, overall anatomy of tissues, pre-surgery preparation, intra operative sutures or post-op care- everything is very different. Over the years, we have developed various steps which should be done to decrease risk of hypospadias surgery complications in adults. This has led to improved results with more than 95% success rate after hypospadias repair with very few adults requiring another surgery.
At Hypospadias Foundation, a dedicated team of surgeons Dr A.K. Singal and Dr Ashwitha Shenoy take care of adult hypospadias. Dr A.K. Singal is a reputed and top hypospadias surgeon who has been doing hypospadias repair surgeries since 2006 and is rated amongst the best in India and the world for his excellent results. Dr Ashwitha Shenoy is a hypospadias surgeon with experience in managing hypospadias. Both work very closely giving best outcomes to adults with hypospadias. Given their teamwork and dedication to success rates in hypospadias, children and adults come from all over India and more than 20 countries to seek hypospadias treatment under their care.