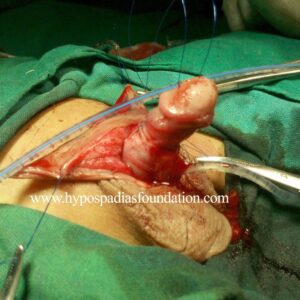
MM, a 35-year male, from Bangladesh a case of failed hypospadias who underwent three hypospadias surgeries in the past but did not get the desired result due to complications of hypospadias repair. He presented to us with complaints of passing urine from two sites – coronal and proximal penile region.
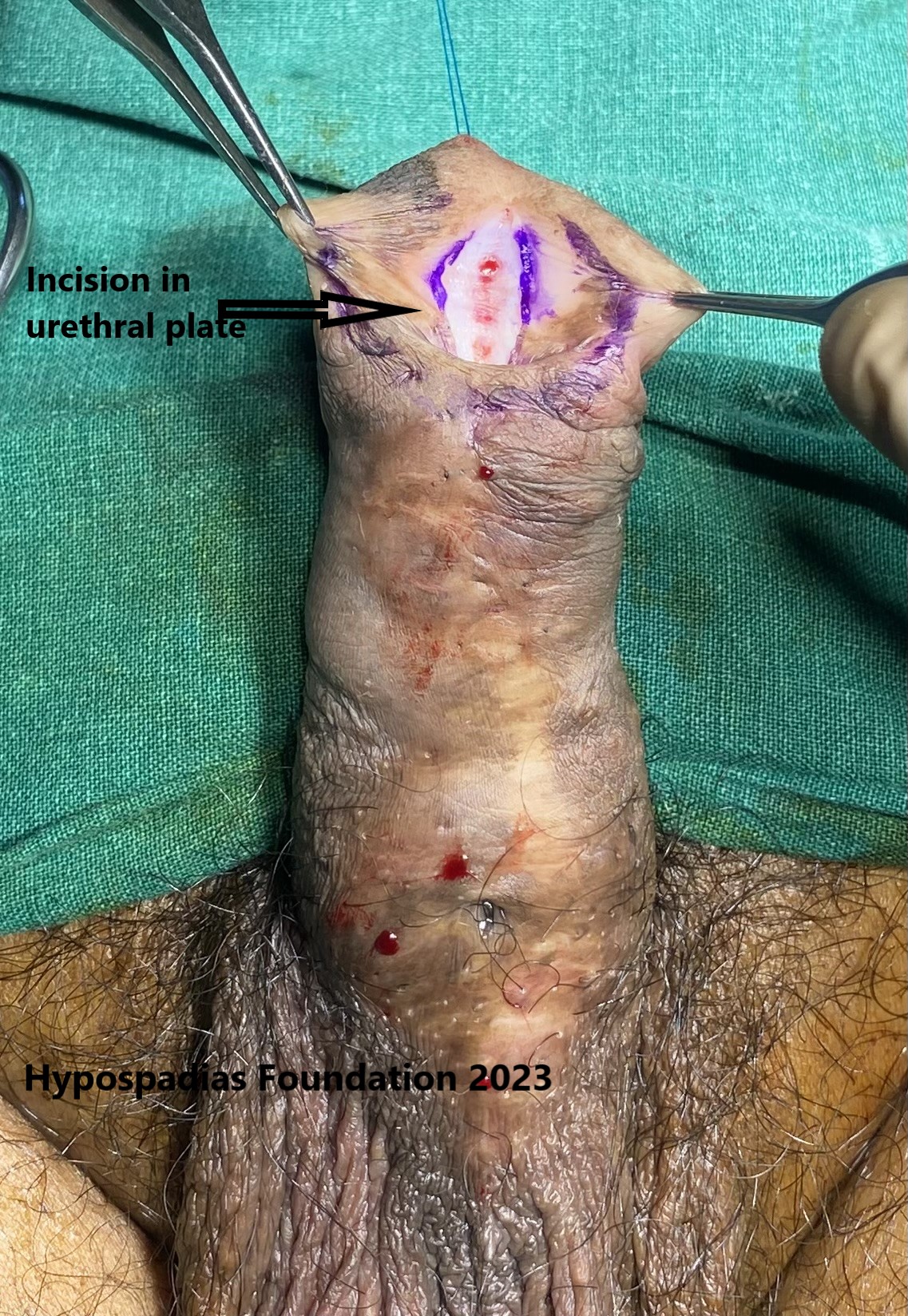
On clinical examination in the OPD, we found that the meatus was located at the coronal region. There was large urethral fistula at the proximal penile region with hair growth from the site of fistula. He was planned for cystoscopy to assess for the status of the urethra and redo hypospadias surgery in a single stage or in two staged was to be decided based on the results of cystoscopy.
1. Clinical picture showing coronal meatus and proximal penile fistula.
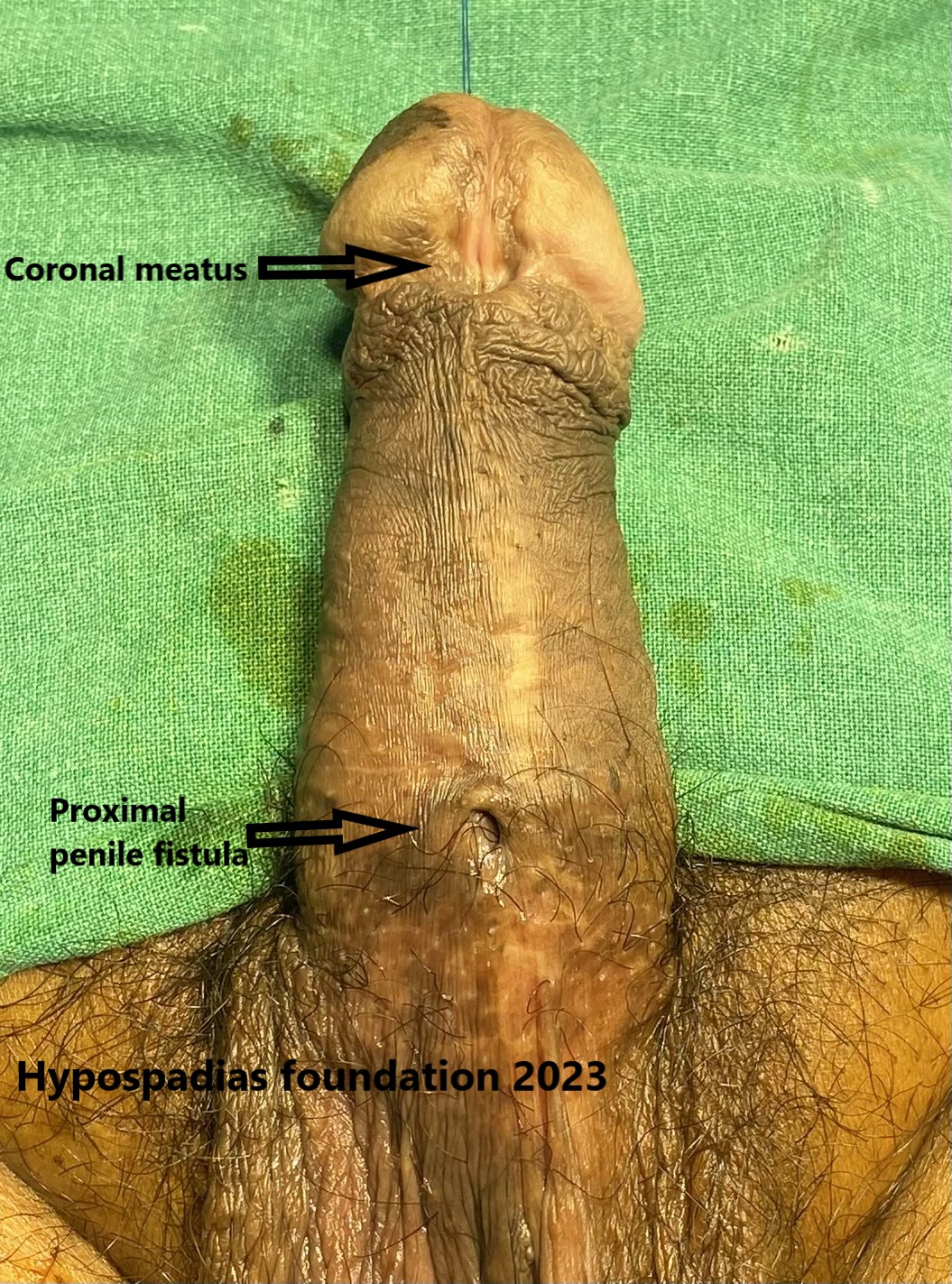
Cystoscopy showed 1cm of hairy urethra at the site of proximal penile fistula, the rest of the proximal urethra was normal. Since majority of the urethra was normal, we planned for single stage repair. We chose to proceed with single stage proximal and distal oral mucosa inlay graft urethroplasty.
2. Cystoscopy picture showing hairy urethra
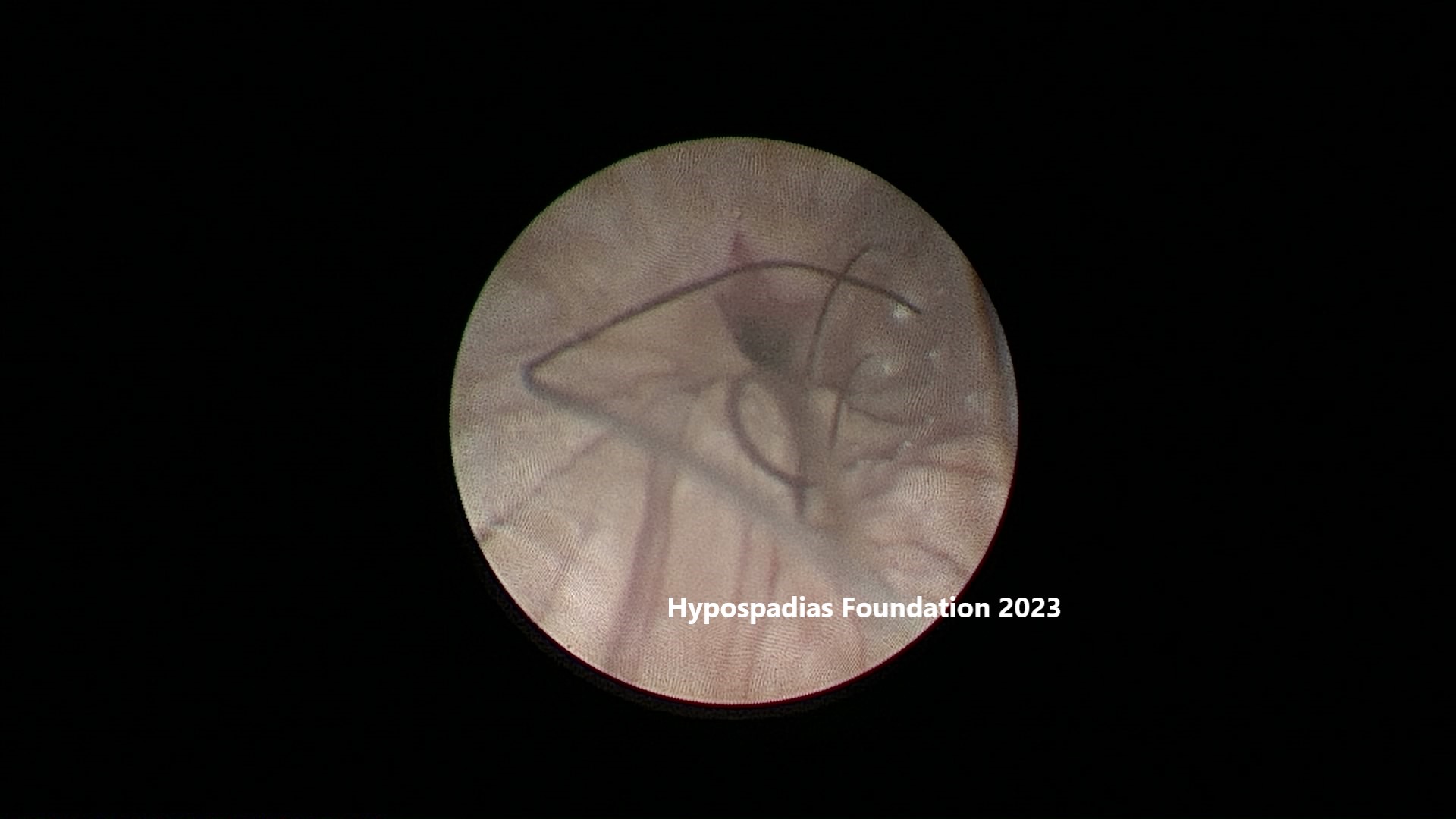
Patient did not have chordee hence degloving was not done. Midline incision was given over the urethral plate in the glans and distal penile region to assess the quality of the urethral plate. The urethral plate was healthy with no signs of scarring. Proximal hair bearing unhealthy urethra was excised completely. Since urethral bed was found to be healthy in the proximal and distal region, we planned to place an oral mucosa inlay graft at both sites and proceed with single stage urethroplasty.
Oral mucosa graft was harvested from the right cheek. The graft was defatted and sutured at the urethral bed distally and proximally. The graft was sutured at the edges of the urethral plate and was quilted in place using 6-0 PDS and 5-0 PDS sutures. Following inlay graft placement, proximal urethroplasty was done using 5-0 vicryl stitch, first layer was continuous subcuticular inverting sutures. Second layer closed using local tissues with 5-0 vicryl. Glans wings were widely mobilized and distal urethroplasty along with Glansplasty was done using 5-0 vicryl.
Patient had a per urethral catheter and suprapubic cystostomy (SPC) after redo hypospadias surgery. Dressing change was done on post operative day 4 and dressing change was done on every 4th day. Per urethral catheter was removed on post operative day 21 and SPC was removed on post operative day 22.
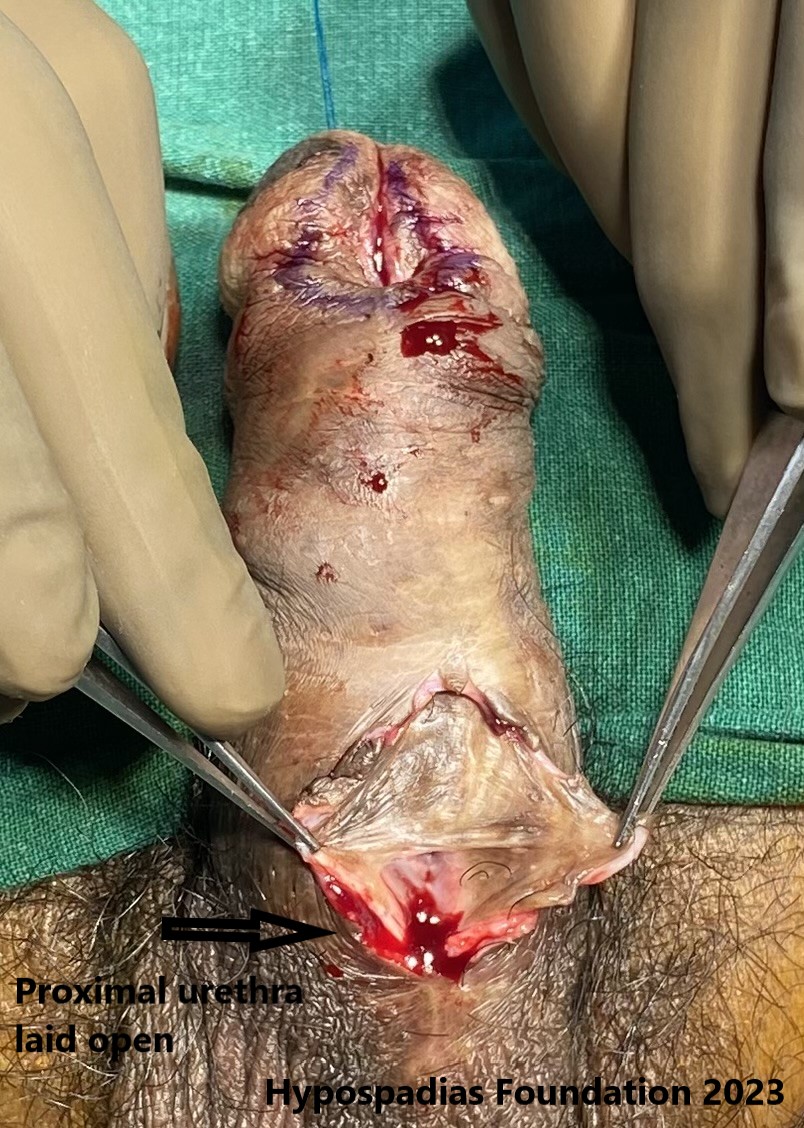
3. a & b Picture shows incision in the distal urethral plate and proximal urethra
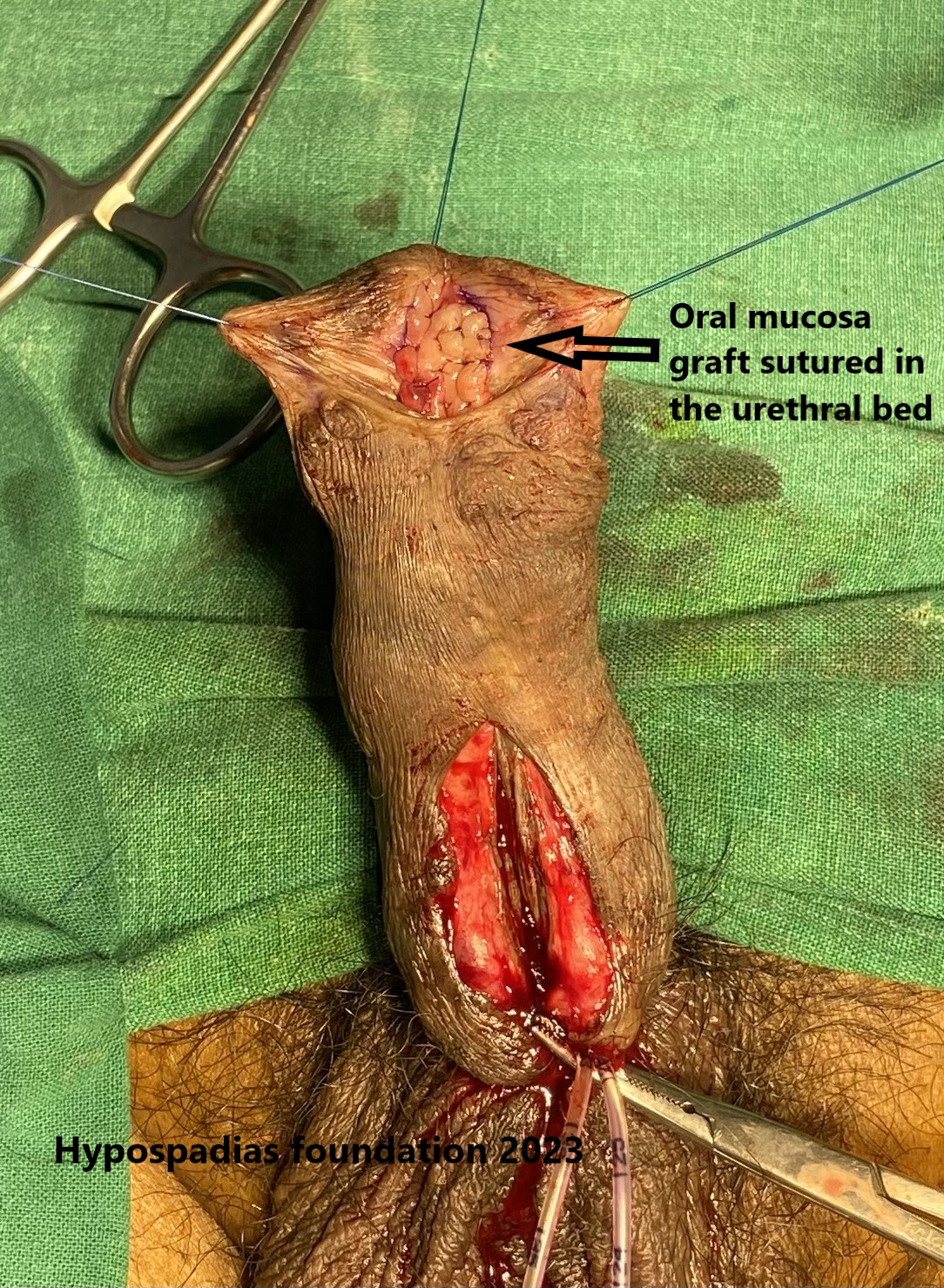
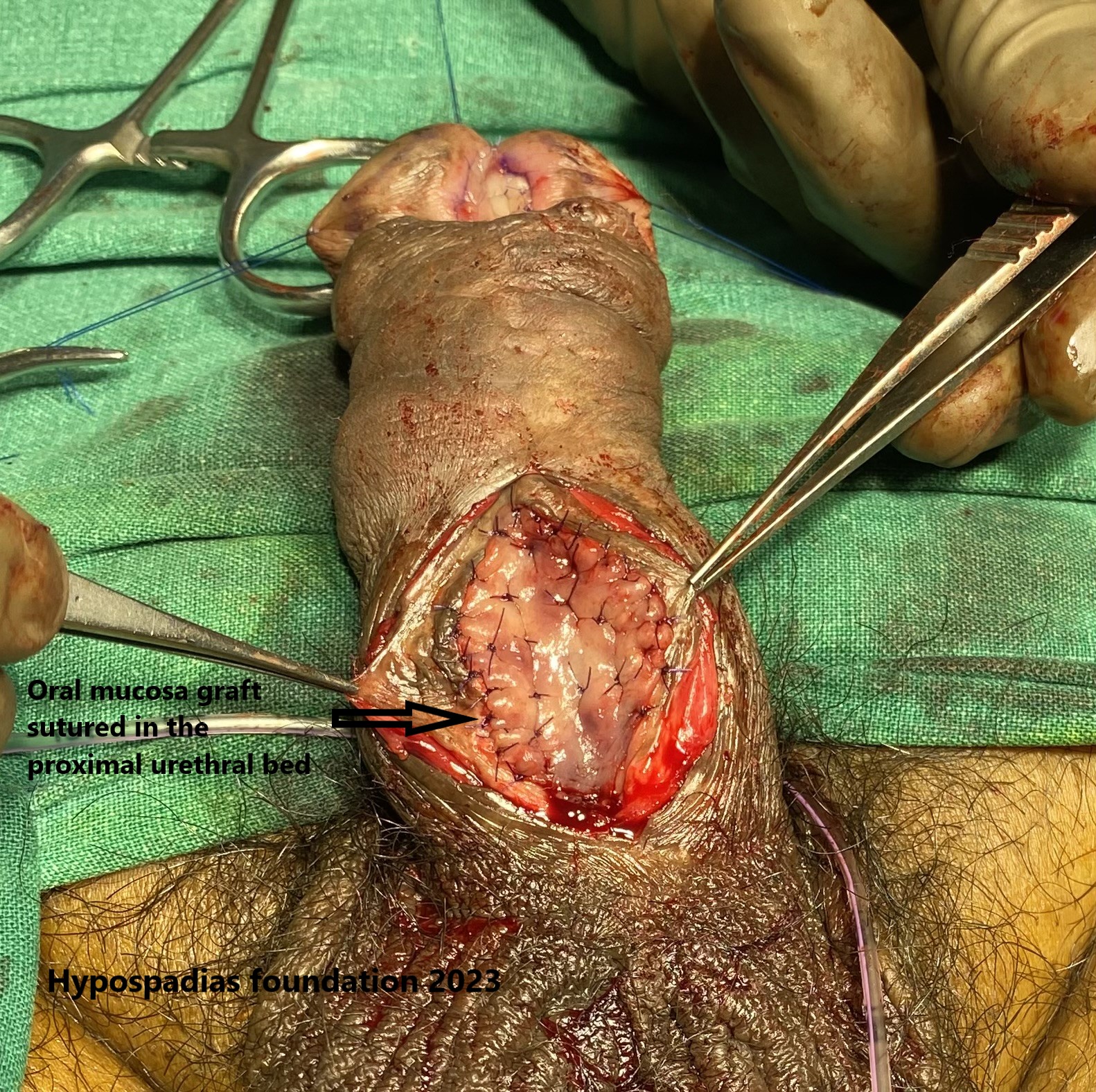
4. a & b Picture showing oral mucosa graft, it has been placed and quilted in the distal and proximal urethral bed


5. a & b: Distal urethroplasty being completed and second picture showing completion of repair both proximal and distal repair

6. Picture showing status at post operative day 15 and second picture shows urine stream after catheter removal.
Patient had a per urethral catheter and suprapubic cystostomy (SPC) after surgery. Dressing change was done on post operative day 4 and dressing change was done on every 4th day. Per urethral catheter was removed on post operative day 21 and SPC was removed on post operative day 22.
Post catheter removal the patient was passing urine in single straight stream with no leak. Patient was started on meatal dilatation using meatal dilator with mild steroid ointment for 3 months.
Redo hypospadias in an adult after previous multiple failed hypospadias surgeries
Hypospadias is commonly diagnosed in childhood, but adults also present with hypospadias because either they were never operated in childhood, or they have complications after multiple hypospadias surgeries in childhood. The common complaints which they present with are poor stream, urinary tract infections, spraying of urine, difficult sexual intercourse, or infertility. The common findings which we find in adults post failed hypospadias repair are hairy urethra, residual chordee, urethral diverticulum or urethral stricture. Most of the adults with these complications will need a redo surgery in either single or multiple stages. In more than 95% of the surgeries, we need to use oral mucosa graft while reconstructing the urethra. It is used either as an inlay graft or in staged repair.
Cystoscopy is the first step in any of these redo hypospadias repairs. Through cystoscopy we will get an idea about the native urethra, presence of any urethral stricture or diverticulum, any hair in the urethra and the diverticulum at the prostatic urethra. This information will help us decide if we can plan a single staged repair or need for a two-stage repair.
In the presence of long segment unhealthy urethra, we may need to plan a staged repair. The unhealthy urethra must be completely removed, and oral mucosa graft should be placed on the urethral bed in first stage and in second stage the urethra is reconstructed from the graft. The second stage is planned when the oral graft over the penis becomes soft like lip and can be easily rolled to form a urethra. The duration between the two stages is somewhere between 6-9 months. If there is short segment of urethra which needs to be replaced, then it can be done in single stage by placing an oral mucosa inlay graft.
The healing in adults after hypospadias repair is slow as compared to children hence per urethral catheter is kept for a longer time which is around 21-28 days. Suprapubic cystostomy is done in every adult undergoing hypospadias urethroplasty. This helps in decreasing the stress on our urethroplasty suture line which in turn contributes to better healing.
About Hypospadias foundation
At hypospadias foundation, we get adults and children from all over the world in search of treatment for hypospadias. We provide support and information for children, adults and their families affected by hypospadias. Dr Singal and Dr Shenoy are deeply devoted to creating awareness and helping patients get the right treatment for hypospadias be it primary, redo or adult hypospadias. Children and adults from more than 25 countries visit our hypospadias foundation in search for cure and are cured of hypospadias.
Dr A K Singal is a highly experienced surgeon and regarded as the best hypospadias surgeon in India and in the world. He has dedicated his life towards treating children and adults with hypospadias. His expertise in this area has helped us achieve excellent outcomes in adults and children with hypospadias.
Dr Ashwitha Shenoy is an expert pediatric surgeon with special interest in pediatric urology and hypospadias. Both Dr Singal and Dr Shenoy work together to give best results for hypospadias surgery in India for both children and adults.
Contact us:
For appointment kindly contact us at the contact details given below.
MITR hospital & Hypospadias Foundation, Kharghar, Navi Mumbai, India – Tue/Saturday 4:00pm-6:00pm, Call for appointments: +91-9324180553. Or email us at hypospadiasfoundationindia@gmail.com
Keywords: best hypospadias surgeon India, Best hypospadias surgeon world, adult hypospadias, redo adult hypospadias, adult hypospadias surgery, adult hypospadias repair, complicated hypospadias repair, hairy urethra, oral mucosa graft repair, oral mucosa inlay graft, failed hypospadias repair, urethral fistula repair, oral mucosa graft urethroplasty, results of hypospadias surgery, failed hypospadias surgery, complications of hypospadias,
If you wish to contact us, pls fill up this form- Contact form for Hypospadias Foundation
or pls call up our clinic for an appointment- https://www.hypospadiasfoundation.com/contact/